What are bacteria or germs?
Bacteria are single-cell microscopic organisms that thrive in diverse environments. They can live in the soil, in the ocean, and inside the human intestine. Human relationships with bacterial cells are complex; sometimes they help by milk clotting and turning it into yogurt, or helping our digestion process. At other times it is devastating, causing diseases such as pneumonia and MRSA. All living organisms - based on the relative complexity of bacterial cells - are broadly classified into eukaryotes and nuclei. Bacteria are protozoan, the entire organism consists of a single cell with a simple internal structure. In contrast to the nuclei of the nucleus, which is carefully packaged in a cell called the nucleus, the bipolar DNA-free ribosomes float freely in a twisted-like mass called the nucleoid.
the structure:
Bacterial cells also contain separate circular pieces of oxygen-deficient ribosome DNA called plasmids. Bacteria lack organelles associated with membranes, the specialized cellular structures designed to carry out a range of cellular functions from energy production to protein transfer. However, both bacterial and microbial cells contain the ribosome. Proteins collect individual amino acids in these spherical units, using information encoded in the pregnant thread (for ribosome-RNA).
Abroad Bacterial cells are generally surrounded by two protective coatings: an external cellular wall and an internal membrane of the cell. However, some bacteria such as mycoplasma do not contain a cellular wall at all. Some bacteria may contain a third protective layer called the capsule. Finally, the bacterial surfaces can be covered by lattice-like extensions (flagella) or cilia. According to Mims Medical Microbiology, long whips help in mobility, while short cilia help bacteria stick to the target surfaces (host).

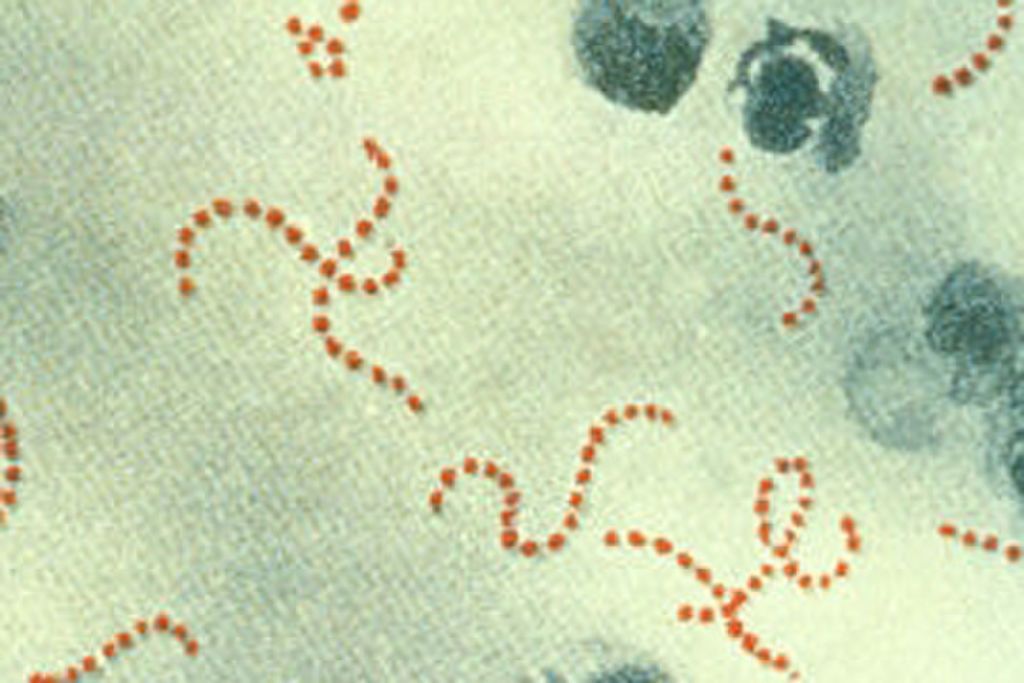
Image description: Bacteria are an eukaryotic, consisting of a single cell with a simple internal structure.
Classification of bacteria:
Some different criteria are used to classify bacteria. They can be distinguished by the nature of their cell walls, their shape, or differences in their genetic makeup. A gram-dye test is used to determine bacteria through cell walls. It was named after Hans Christiangram, who developed the technique in 1884.
The bacteria first form a purple pigment called crystalline violets, which are particularly related to peptidoglycans, a complex structure of amino acids and sugars found in the cell wall. This is followed by a series of steps that eventually lead to the removal of the unrestricted or weakly restricted crystal violets. The cells are then dyed with a red dye called porcupine.
Gram-positive bacteria pigment purple because their cell walls are rich in peptidoglycans. On the other hand, Gram-negative bacteria in which cell walls contain two layers take red.
The outer layer of fat is not strongly linked to crystal violet and the dye is easily washed during the dyeing process. For example, pulmonary streptococcus that causes pneumonia is a Gram-positive bacterium, whereas E. coli and cholera hemorrhagic cholera are gram negative bacteria.
There are three basic forms of bacteria, according to Mims Medical Microbiology. Circular bacteria are referred to as macrophages (monoclonal) and to cylindrical bacteria in the form of capsules (single-rodent), while sporadic bacteria are referred to as helical. Staphylococcus can also be joined together in different images: a group of two or double, ring, streptococcal, staphylococcus or staphylococcus aureus.
The forms and configurations of bacteria are often reflected in their names. For example, the acid-lactic acid-laden bacteria are the bacilli, the pneumococcal pneumonia that causes pneumonia is a series of staphylococcus. The classification criteria mentioned so far are based on physiological and morphological characteristics. However, bacteria are classified on the basis of their evolutionary relationships to each other, ie drawing a type of family tree for all bacterial species, is a relatively new development.
This type of evolutionary classification was made possible with the advent of nucleotide sequencing (the ability to read the nucleotide arrangement in oxygen-deficient ribosome DNA or ribosome DNA). Since ribosomes exist in all living organisms, one can look at similarities and differences in ribosome DNA sequences that encode specific ribosomal proteins and determine the degree of association of different organisms.
In his article, "How We Look and Look and How We Should Look at Bacteria and Microbiology" - which includes "Epidemiology, Third Edition, Vol. 1" (Springer, 2006), Carl and Weiss noted that the sequence (rPNA) A clear concept of bacteria by spreading the relationships of evolution between species.
Using the early sequencing technique developed by Frederick Sanger in the mid-1960s, Weiss began to distinguish ribosome ribosome DNA and discovered a second group of rudimentary organisms called macrophages (a group of microbes that are different from known microbes in terms of molecular structure). Until then, the only known members of this group - methane generators - had mistakenly identified them as bacteria. In 1977, Woz and George Fox, published in PNAS, reported that methane generators do not carry a "tissue resemblance" with bacteria.
Reproduction:
Most bacteria reproduce in a process called binary fission. One bacterial cell, the mother cell, makes a copy of its oxygen-deficient ribosome DNA and grows in large size by doubling its cellular content. The double contents are pushed to any end of the cell, and then a small cleavage appears in the middle of the mother cell, eventually dividing it into two identical cells (the daughter cell). Some bacterial species - blue bacteria (zebras, bacteria that live in water and produce energy through photosynthesis) and wall stabilizers - thrive through budding. The new cell grows during budding as a branch of the mother cell. Start like a small knot, grow up to be the same size as the mother, and break down.
The ribosome DNA in the mother and progenitor cells is identical to the bifurcation or budding, so the bacterial cells try to introduce some variation in their genetic material by merging the extra oxygen-deficient ribosome DNA into their genome. This is known as the horizontal transfer of the gene, and the resulting genetic variation ensures that bacteria are able to adapt and survive as their environment changes. This happens in three ways: transformation, transport, and coupling.
During conversion, bacterial cells integrate small parts of the oxygen-deficient ribosome DNA from its surrounding environment. According to the source, these fragments (small parts) may be released by neighboring bacteria that have been torn apart.
On the other hand, transport occurs when bacteria become infected with special viruses known as bacteriophages or bacteriophages, which can carry the ribosome-deficient bipolar DNA.
Pairing requires physical contact between two types of bacteria. Genetic material - usually a double plasmid - will move from donor to recipient. This plasmid version travels out through a physical extension called cilia, and enters the receiving bacterial cell. The donor bacteria contain a sequence of the oxygen-deficient ribosome called F (factor F), which enables the formation of cilia. Coupling can help spread antibiotic-resistant genes.
Bacteria in human health and disease:
Bacteria can be beneficial and also harmful to human health. Bacteria that share the range and resources within our bodies tend to be useful. David A. "There are more than 10 times more bacterial cells than human cells in the human body," said Reelman, a specialist in microbiology at Stanford University in a 2012 article in Nature. The largest number of microbial species were found in the gastrointestinal tract.
The human intestine is a comfortable environment for bacteria, with many nutrients available for its application. In an article entitled "Human Microbiology Analysis: A Guide to Doctors in the American Journal of Gastroenterology, the researchers reported that intestinal bacteria and other microorganisms help digestion, avoid colonization by harmful pathogens, and help develop the immune system .
Furthermore, gastrointestinal disturbance has been associated with some pathological conditions. For example, patients with Crohn's disease have increased antibodies against intestinal bacteria and white blood cells are highly aggressive towards antibiotics, according to researchers in the article "Gut Flora in Health and Disease," published in The Lancet in 2003.
Other bacteria can cause infection. For example, Streptococcus pneumoniae causes pneumonia. Several types of bacteria, ranging from Group A, Streptococcus, Clostridium, Escherichia coli and Golden Staphylococcus aureus, can cause a rare but severe infection in soft tissue, called necrosis fascia, sometimes called "carnivorous bacteria". According to Centers for Disease Control, these infections affect tissues surrounding muscles, nerves, fat and blood vessels but can be treated, especially when discovered early.
Antibiotic resistance:
Antibiotics are usually used to treat bacterial infections. But in recent years, improper or unnecessary use of antibiotics has led to the proliferation of many strains of antibiotic-resistant bacteria.
Antibiotic resistance is a phenomenon in which infectious bacteria are no longer affected by the effective antibiotics that have been previously addressed. According to the CDC, at least two million people are resistant to antibiotics every year in the United States, resulting in at least 23,000 deaths each year.
"I have identified any infection that you can think of now as linked to a level of resistance," said Dr. Christopher Krenich, a infectious disease and epidemiology doctor at the University of Wisconsin and Madison Hospitals. There are very few infections that we treat now as long as the infection caused by resistance bacteria is not a medical concern. "
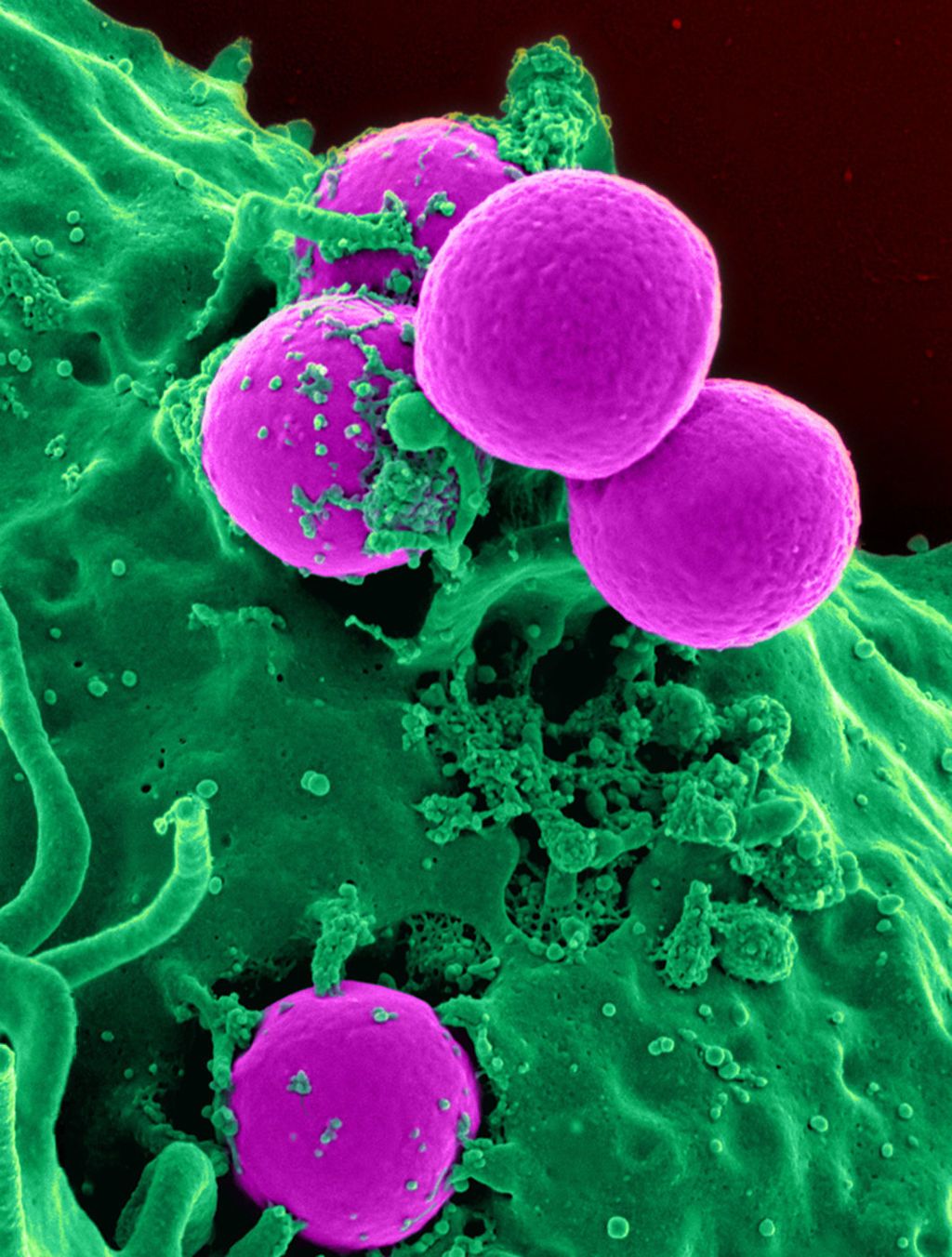
One of the most common bacterial strains resistant to known antibiotics is methicillin-resistant staphylococcus aureus, which resists methicillin and other antibiotics used to treat Staphylococcus infection. It spreads primarily through skin contact.
Methicillin-resistant Staphylococcus aureus occurs in health care settings such as hospitals and nursing homes, which can lead to pneumonia or a bloodstream infection. This germ is also spread in society, especially in cases where there is a lot of skin contact or the use of common tools. For example among athletes, in tattoo salons, or in day care facilities and schools. Staphylococcus aureus-resistant Staphylococcus aureus infection often causes skin infection.
An important aspect of antibiotic resistance is to be cautious about its use. "It's very important for us to use antibiotics smartly," he told LiveScience. "You just want to use an antibiotic when you have a clear bacterial infection."
Source : Live Science








0 Comments